Dental bone grafting rebuilds or replaces jaw bone to support teeth, implants, or to repair damage. This overview on dental bone grafting explains what it is, why it’s done, common procedures, risks, costs, and questions to ask your dentist.
What is dental bone grafting?
Dental bone grafting is a surgical procedure that adds bone or bone-like material to the jaw. Grafts restore lost volume and shape, support dental implants, and help stabilize surrounding teeth and tissues after injury, disease, or long-term tooth loss.
Common reasons patients need dental bone grafting
Patients often need grafts after tooth extraction, advanced periodontal (gum) disease, facial trauma, or when teeth have been missing for years and bone has resorbed. A low sinus floor in the upper back jaw can also make a graft necessary before implants.
Types of graft materials used in dental bone grafting
Autograft
Autografts use the patient’s own bone taken from another site, like the chin or hip. Pros: best biological match and healing potential. Cons: extra surgical site, more discomfort and slightly longer recovery.
Allograft, xenograft, and synthetic grafts
Allografts come from human donors, xenografts from animals (usually bovine), and synthetics are lab-made materials. These options avoid a second surgical site and are commonly used when ample donor bone isn’t available. Choice depends on case needs and surgeon preference.
Common dental bone grafting procedures
Socket preservation
Placed at the time of extraction, this maintains the socket shape and preserves bone for future implant placement.
Ridge augmentation and block grafts
Used to rebuild lost jaw width or height. Block grafts use a solid piece of bone to replace substantial defects.
Sinus lift
A sinus lift raises the sinus membrane and places graft material in the upper back jaw to create enough height for implants.
What to expect before, during, and after surgery
Planning typically includes an exam and 3D imaging (CBCT) to map bone and anatomy. Surgery is done under local anesthesia with sedation options. Afterward expect swelling, mild pain, and a soft-food diet for a few days. Healing often takes several months before implant placement; follow-up visits monitor integration.
Risks, benefits, and factors that affect success
Benefits include a stable foundation for implants and better long-term oral health. Risks include infection, graft failure, or prolonged swelling. Success is higher with good oral hygiene, controlled medical conditions, and avoiding smoking.
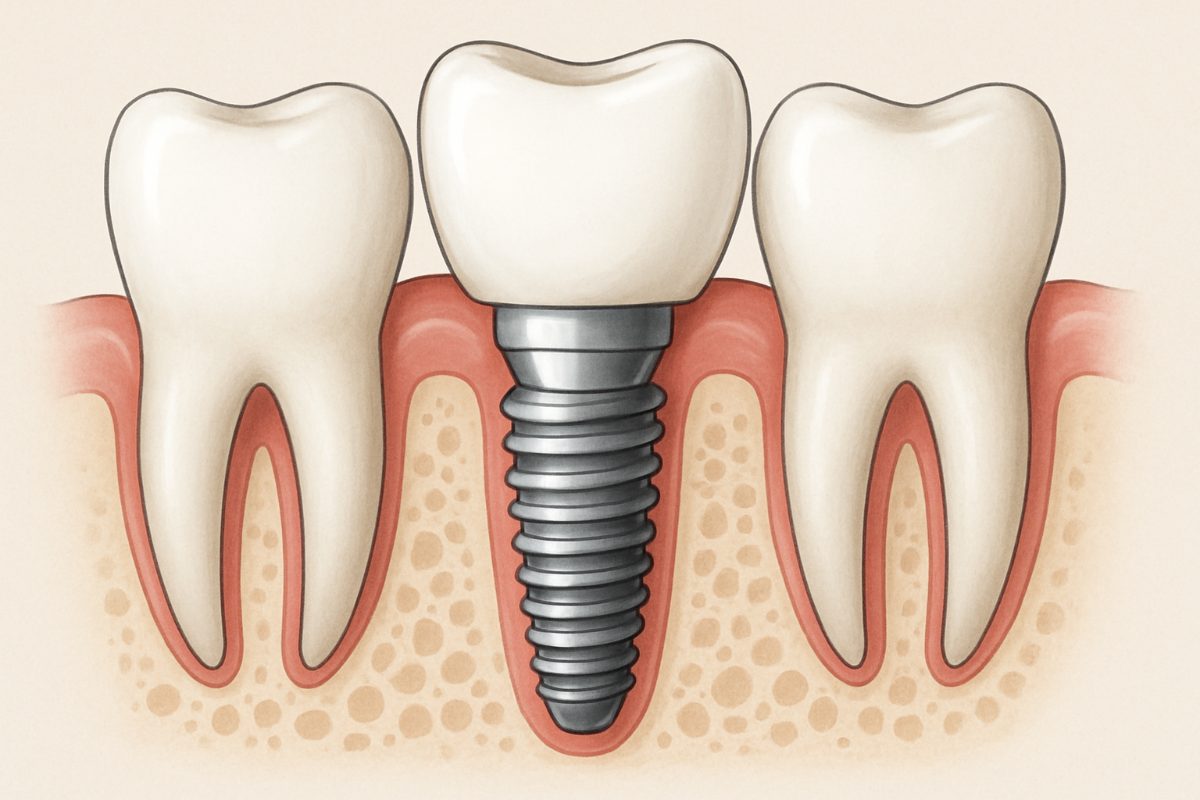
How dental bone grafting fits into implant treatment plans
Grafting can be a staged step before implants or done at the same time, depending on bone volume and surgical goals. Proper grafting increases the chance of long-term implant success and allows for better implant positioning and esthetics.
Typical costs and financing options
Costs vary by graft type, surgical complexity, imaging, and anesthesia. Insurance coverage is inconsistent. Many practices offer financing or payment plans to spread cost—ask about options like CareCredit or other third-party plans.
Questions to ask your dentist about dental bone grafting
Ask what graft material will be used, who will perform the surgery, which imaging tests are needed, expected healing time, success rates for your case, and alternatives if grafting isn’t recommended.
Why choose MoArk Dental & Implants for dental bone grafting
MoArk Dental & Implants provides same-location care from 3D diagnostics to restoration, making coordination simple. Their team uses CBCT imaging, digital planning, and an on-site lab for fast, precise results. Experienced doctors and modern tools support predictable grafting and implant outcomes.
Next steps and scheduling a consultation
To learn if dental bone grafting is right for you, schedule a consult and bring any recent dental records or X-rays. A thorough exam and 3D scan will clarify your options and next steps toward a stable, long-lasting restoration.